Rosemary Apol-Hoezee is director of quality and education for Holland Home, a continuous-care organization in Grand Rapids, Michigan. Part of her job involves training caregivers to provide the best evidence-based care for people with dementia. Apol-Hoezee has been a mental health nurse in geriatric and general populations and has a Master of Public Health degree. In this edited conversation, she explains how church members can learn to engage and include people living with dementia and their caregivers.
What do you hear from caregivers and family members of those who live with dementia?
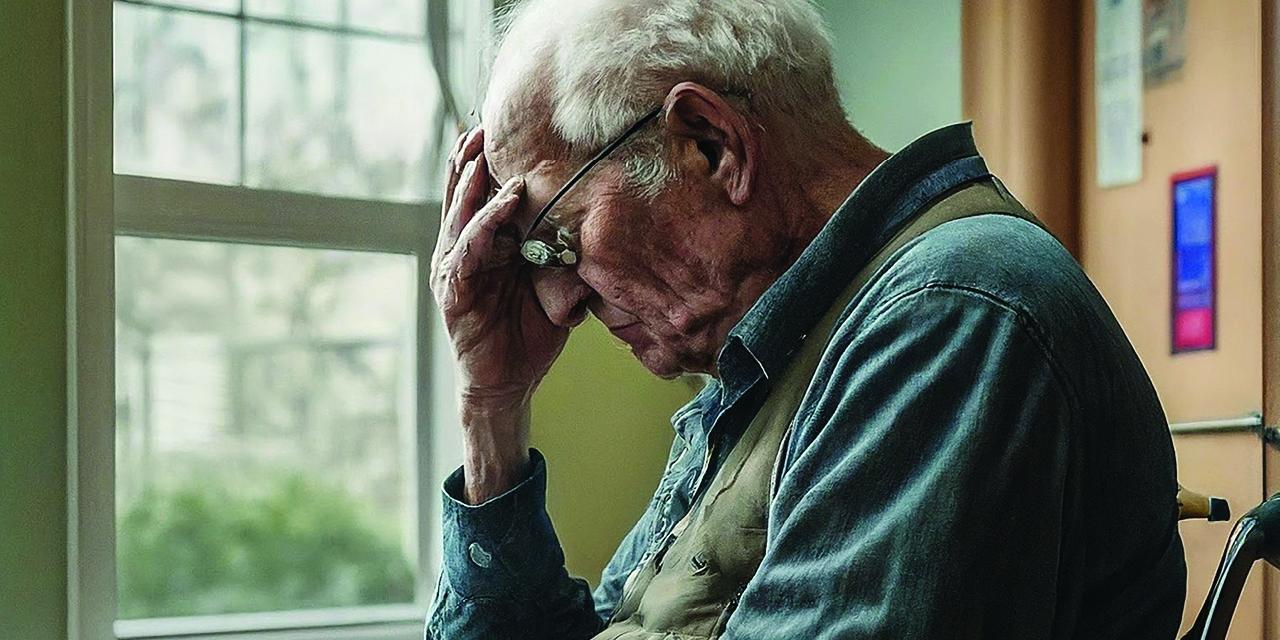
In support groups I facilitate, caregivers talk about feeling lonely and isolated: “We don’t hear from our friends anymore. People don’t know how to relate to someone with dementia.” This uncertainty often prevents church members from talking at church with those who have dementia, visiting them at home or in care facilities, or offering respite care.
Who influenced your current approach to dementia?
We have learned so much more about dementia thanks to our collaboration with Teepa Snow. She is a world-renowned dementia care specialist who founded Positive Approach to Care (PAC). In 2016, I and my co-worker Lynn Bolt, a nurse educator, attended an intensive PAC training that changed our lives and careers. It led to our Holland Home staff becoming PAC trained so that they would be able to provide evidence-based care to people living with dementia.
One of the main insights is how important the value of connection is. Teepa Snow teaches that caring for people who live with dementia is all about developing a relationship with each individual. Her GEMS model focuses on what people can still do as dementia progresses. She talks about different brain states, rather than disease stages, because symptoms can vary throughout the day. Understanding the changing brain states helps us reduce distress and look for opportunities for interaction that have meaning and value.
What would you like clergy and congregations to know about dementia?
I’ve heard from clergy who believe that every worship service for people with dementia must mention sin and include an altar call. Some clergy believe that people who’ve lost a certain amount of cognition should no longer take part in the Lord’s Supper because they can’t properly discern the Lord’s body. I’d like clergy and congregations to know that even if a person’s brain changes, God still sees them as precious and unique.
Different diseases and symptoms fall under the umbrella term “dementia.” We now know that fairly early on in dementia, people lose one out of every four words. That means every fourth word they hear is incomprehensible. People lose about 40 percent of peripheral vision early in the disease. We are seeing more early-onset dementia among people in their sixties. The five senses become muted, but, even when they have a harder time speaking or understanding words, people with dementia still notice sensations and how things feel.
Why can church worship be difficult for lifelong churchgoers who lose cognitive abilities?
Being exposed by the Calvin Institute of Christian Worship to disabilities experts like the late Barbara J. Newman, Victoria White, and LaTonya McIver Penny has made me think about how restrictive or exclusive worship services can be. I’m a literary person and appreciate well-crafted sermons, but some people can’t process all those words.
Some church traditions place a high emphasis on quiet and reverence, so, if a person with dementia stands up, walks around, or responds during the homily, the people around them think they’re being disrespectful. They might shush the person. Even fully cognizant adults who struggle with ADHD might be helped if they have something to fidget with. Many caregivers stop going to worship services for fear their loved may be an embarrassment in worship. These caregivers really need the comfort of worship but have no one else to sit with or stay home with their loved one.
How have you helped clergy or church councils learn more about dementia?
Lynn Bolt and I have given presentations to clergy and councils about how dementia affects brains and how skills and techniques can help people better relate to those with dementia. When we showed PET scans of healthy brains and those affected by dementia, we were impressed by how many people said, “I had no idea how their vision or language comprehension and production changes!”
For example, if you give what you think of as a friendly touch to someone who can’t see you coming, their brain may perceive it as a threat. They may startle, jump, or even cry out because your touch evoked their fight or flight response. And then they are perceived as disruptive.
How might you encourage fellow church members to talk with people with dementia at church or in memory care facilities?
Teepa Snow teaches a very specific process, starting with being mindful of public, personal, and intimate space. Don’t approach someone from the side. Stand about six feet away and in front of them to give a visual cue. Put your hand by your face, smile, and say something like, “Hi, my name’s Rosemary and you are John DeVries.” Slowly hold out your hand and see whether they reciprocate. Give them a special hand-under-hand handshake. Then move to their side and sit beside them at eye level. Be friendly and give compliments. Keep your message short, simple, and friendly. What matters most is that you use the person’s name and show warmth.
You’ve helped plan the second edition of the Evening Star worship handbook.
Yes, in 2003, Holland Home had a worship renewal grant from Calvin Institute of Christian Worship to explore how to meet spiritual needs of dementia care residents. A revised edition of Evening Star: Worship Ministry for Persons Living with Dementia, Handbook for Worship is available for purchase.
We’ve worked hard to make this a manual that either a clergyperson or a layperson could use. We want non-pastors to feel comfortable leading a service in a memory care residence if they choose to do so. Besides including more content about how brains change with dementia, the second edition explains how those changes affect the way we craft the worship services, how we speak, the words we use, and so on.
Learn More
Watch Holland Home’s brief “Dementia Journey” video (7 min., 15 sec.) to get an immersive sense of what dementia feels like. Download Holland Home’s Dementia Care Handbook, which describes Teepa Snow’s GEMS model (pp. 18–24). Gather a group to read and discuss Second Forgetting: Remembering the Power of the Gospel During Alzheimer’s Disease, by Benjamin T. Mast, or Dementia Guide for Faith Communities and Leaders, by Rev. Linn Possell and Teepa Snow.